Research Interests
Nutrition is a foundational determinant of immune health, directly shaping how the body defends against disease and regulates inflammation. Malnutrition, whether due to deficiencies or imbalances in essential nutrients, can impair immune responses and the severity of infections and allergic diseases. By understanding the interplay between dietary components and immune cell metabolism, we can develop targeted nutritional strategies to prevent and treat immune-driven conditions such as asthma and allergies, highlighting the crucial role nutrition science plays in advancing respiratory and overall health.
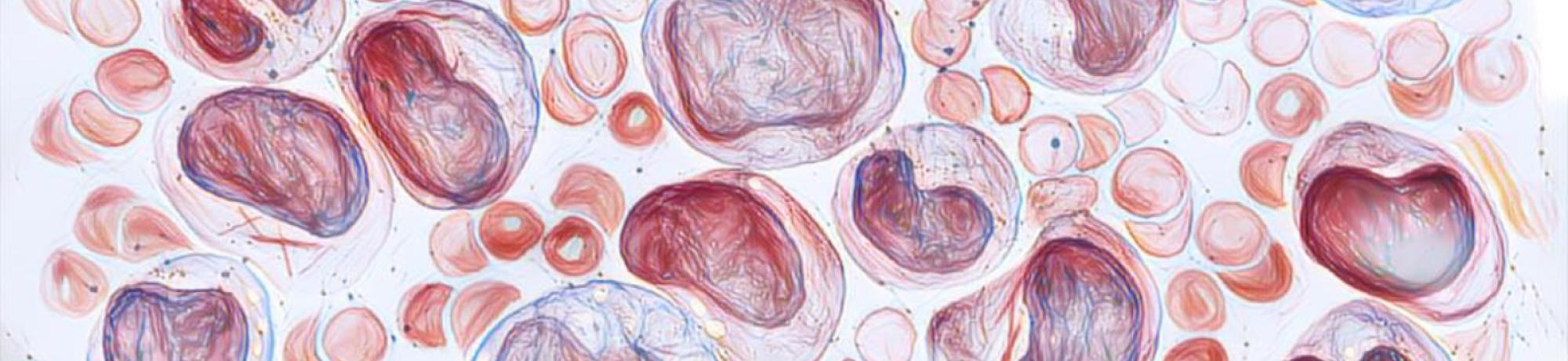
Our laboratory is dedicated to uncovering how nutrition and metabolism influence immune cell development and function, with a special focus on asthma and allergy. By targeting the metabolism of various immune cells through specific dietary components — such as micronutrients and amino acids — we investigate how tailored nutritional interventions can shape immune responses. Our research spans a range of immune cell types, with particular expertise in T cells, innate lymphoid cells (especially ILC2s), and granulocytes, allowing us to uncover cell-specific metabolic pathways that can be strategically targeted to improve immune balance and respiratory health. Our research integrates diverse cutting-edge mouse models, including genetically modified strains, customized diets and established asthma models, to dissect how dietary factors influence immune function and asthma pathogenesis. Combining flow cytometry, transcriptomics, and metabolomics, we analyze immune cell populations and their metabolic states, with a particular focus on oxidative phosphorylation (OXPHOS) as a critical energy pathway in immune cell activation.
Iron as a key regulator of ILC2-mediated asthma
Our research has established that iron is essential for the proper function of ILC2s, key drivers of allergic inflammation in asthma. We have shown that iron supports multiple metabolic processes in ILC2s, enabling their activation and cytokine production. Central to this is the mitochondria, the powerhouse of the cell, which plays a critical role in fueling immune cell function through iron-dependent pathways like OXPHOS. Because iron is also vital for systemic functions like oxygen transport, our focus is on developing strategies to modulate iron availability specifically within ILC2s, but without disrupting overall iron homeostasis. By precisely targeting iron uptake and mitochondrial metabolism in ILC2s, we aim to reduce airway inflammation and improve asthma outcomes while preserving essential iron-dependent processes in the rest of the body.
New molecular checkpoints in ILC2 function
- Ligand-receptor pathways. Our laboratory is focused on identifying novel modulators of ILC2 function that influence their activation and immune responses. We are particularly interested in molecules and pathways that, like certain key ligand-receptor interactions involved in immune regulation, can modulate ILC2 activity without broadly affecting other cell types. We are especially interested in molecules and pathways such as specific cytokines, chemicals, or co-stimulatory molecules. By exploring how these modulators impact ILC2 metabolism, signaling, and cytokine production, we aim to uncover new mechanisms that could be targeted to control allergic inflammation and improve respiratory health.
- Nutrient-driven pathways. We are interested in identifying dietary factors that modulate the function of ILC2s. Building on our discovery that iron and calcium are crucial for ILC2 activation and metabolic function, we are now expanding our efforts to explore a broader range of nutrients — including amino acids, minerals, and other dietary components — that may serve as novel regulators of ILC2 responses. Using cutting-edge immunology tools — including high-parameter flow cytometry, metabolomics, transcriptomics, and mitochondrial functional assays — alongside advanced ex vivo models and targeted dietary interventions, we aim to dissect how specific nutrients shape ILC2 activation and lung pathology.
Nutrition and lung inflammation
Beyond focusing on ILC2-driven inflammation, our research also explores the role of other key immune cells such as T cells and neutrophils in lung inflammation. Neutrophilic asthma and acute respiratory distress syndrome (ARDS) are characterized by excessive neutrophil accumulation, which contributes to airway damage and inflammation. Neutrophils have a particularly high demand for nutrients such as iron, more so than any other immune cell, to sustain their rapid activation and function. We aim to understand how nutrients influence these diverse immune populations and their metabolic pathways, ultimately seeking new nutritional strategies to modulate neutrophilic and T cell–driven lung inflammation and improve respiratory outcomes.